A late-December Nipah virus outbreak in India’s West Bengal, involving two infected healthcare workers, has raised worldwide concern.
With a mortality rate in the range of 40 to 75 percent, Nipah, a zoonotic pathogen, with fruit-eating bats and animals such as pigs being its primary host, has no available cure.
The virus transmits through contaminated food as well as person-to-person contact, with an incubation period of four to fourteen days. This has led some of India’s neighboring countries to impose COVID-like screening measures at airports.
India’s health ministry said in a statement on Tuesday, January 27, that 196 people who were in contact with the two patients have been traced and tested.
Doctor details how Nipah spreads and how the most vulnerable can be careful amid tightened airport protocols

Image credits: Suvarnabhumi Airport
According to the Indian health ministry, no new cases were detected in the precautionary tracing and testing.
One of the two positive cases has recovered, with the other being in critical condition, the department further confirmed.

Image credits: Suvarnabhumi Airport
Dr. Seethu Ponnu Thampi, a community medicine expert and an assistant surgeon with the Kerala Health Service Department, said in a statement to The National that authorities will seek to cut the chain of transmission as soon as possible.
Dr. Thampi’s contribution to containing the Nipah virus outbreak in Kerala, India, in 2018 was depicted in the 2019 Malayalam thriller Virus.

Image credits: 7NEWS Australia
Symptoms of the virus include fever, headache, muscle pain, vomiting, and sore throat. This can be followed by dizziness, altered consciousness, acute encephalitis, and severe respiratory problems.
Healthcare personnel are at high risk of contracting the virus due to their proximity to symptomatic patients.
Here is how to avoid the Nipah virus
Image credits: hopefloats2019
Image credits: NIAID
Those working in the medical field should adhere to preventative measures such as using gloves, face masks, and goggles, and, if possible, don full PPE (personal protective equipment) kits when dealing with suspected cases.
The general population should avoid areas with lush greenery where fruit-eating bats are likely to gather.
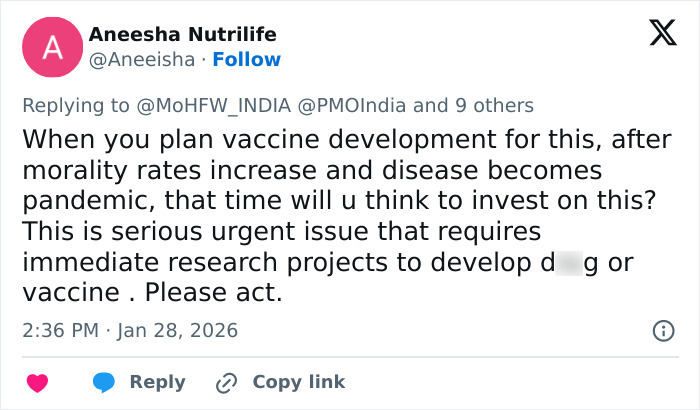
Image credits: Aneeisha
Handwashing and isolation upon symptom onset, much like during the COVID-19 pandemic, can prove crucial in stopping the spread of Nipah.
India’s neighbors have moved to strengthen screening measures at airports
Image credits: MoHFW_INDIA
Singapore’s Communicable Diseases Agency said in a statement on Wednesday, January 28, that it will set up temperature screening at its airport for flights arriving from affected areas of India.
“We are also reaching out to our counterparts in South Asia to better understand the situation. Work is ongoing to establish a global platform for countries to report genome sequencing of detected cases,” the statement added.
Hong Kong has also imposed temperature checks for passengers arriving from India.

Image credits: onmanorama
Malaysia has informed of similar preparedness against the virus, alongside Nepal, which will need to assess risk not only at its airport but also at the land border points it shares with India.
Thailand has assigned restricted parking for aircraft arriving from the country, with its health ministry saying passengers must complete health declarations before clearing immigration.

Image credits: ambquinn
No Nipah virus cases were detected in China as of late Tuesday, according to an official confirmation by the country’s National Disease Control and Prevention Administration.
The risk of imported cases, however, remains high as China gears up to welcome returning nationals and tourists for the upcoming Lunar New Year.
WHO views Nipah as an epidemic-inducing virus
Image credits: dsuperrboy

Image credits: Ken Chuang (Not the actual photo)
The Nipah virus is grouped by the World Health Organization alongside pathogens such as COVID-19 and Zika because of its potential to trigger a pandemic.
The institution lists Nipah among its top ten priority diseases and has included it in its R&D Blueprint for Epidemics, a global plan aimed at speeding up the development of critical countermeasures such as vaccines, diagnostic tests, and medications.
There is currently no vaccine for Nipah. Treatment relies on intensive care and symptom management to improve survival.
First identified 25 years ago, Nipah has repeatedly proven to be life-threatening

Image credits: w4termeloncat
Image credits: CammVilenc76928
The first recognized outbreak of Nipah occurred in September 1998 among pig farmers in Malaysia. The virus is named after the village where it was first identified.
A total of 265 cases of acute encephalitis were reported at the time, resulting in 105 casualties. One million pigs were culled in an effort to contain the virus.
Nipah spread from Malaysia to Singapore in early 1999, with 11 cases and one fatality recorded in the country.

Image credits: TheInsiderPaper
Bangladesh has borne the brunt of Nipah since 2001, with 347 cases recorded until September 2025 and a fatality rate of 71.7 percent.
Nipah first reached India in 2001, taking 45 lives in Siliguri, West Bengal, after infecting 66 people. In 2007, the virus struck the state again, claiming all five people it infected.
Kerala became the Nipah hotspot in India in 2018, resulting in 17 deaths among 19 cases.
Following the late 2025 outbreak in West Bengal, India’s health ministry said it is closely monitoring the situation with “all necessary public health measures” in place.
“Lockdown 2.0 incoming,” a netizen commented about the Nipah outbreak